Approximately 40-80% of people complain that the vertebrae in the lumbar region pain, but not more than 25% of them seek medical help. In fact, the unpleasant sensation that can be caused by both reasons are quite harmless and pathological changes in the spine. Therefore, you should not treat them with contempt.
Causes of back pain
The spine is made up of a whole complex of structural elements: bones, joints, intervertebral discs, ligaments, nerves. Changes in any of them may be accompanied by painful sensations, and of different nature. In addition, the spinal column is surrounded by paravertebral muscles, pain in which patients often confuse with pain in the spine. Therefore, the causes of pain can be many. This can be too much work, the natural rearrangement of the body during pregnancy, and others. But if the pain occurs regularly, it is worth contacting a vertebrologist or neurologist, because often the fact that the spine is systematically painful in the lumbar region indicates the development of certain diseases.
Often, in such cases, patients are diagnosed with:
- intervertebral disc pathology (decreased disc height, protrusion, intervertebral hernia, diskitis);
- facet joint pathology (spondyloarthrosis, joint cysts);
- inflammatory diseases (ankylosing spondylitis or ankylosing spondylitis, reactive arthritis, psoriatic arthritis)
- vertebral compression fractures against the background of osteoporosis;
- neoplastic lesions of the spine.
Pathology of the intervertebral disc
Degenerative changes in the intervertebral disc or osteochondrosis are very common, especially in young and middle -aged people. This is largely due to the need to sit for long periods or engage in heavy physical labor. In old age, the discs dry out and the vertebrae grow together.
Already in the early stages of the onset of degenerative changes in the intervertebral disc, which is a special configuration cartilage that divides the vertebral body, pain in the spine may occur. This is due to irritation of the pain receptors of the outer layer of the disc, as well as the posterior longitudinal ligaments of the spine. Often, osteochondrosis provokes an aseptic inflammatory process, which leads to reflex spasm of segmental muscles. As a result, pain in the spine increases, and there is also a restriction on mobility.
Osteochondrosis tends to constantly progress, especially in the absence of appropriate treatment and lifestyle corrections. Thereafter, it leads to the formation of protrusions, and then to the intervertebral hernia, which gives rise to the severity of existing symptoms and the appearance of new ones.
The lumbar region, due to the fact that it carries the highest load in daily activities, is most often affected.
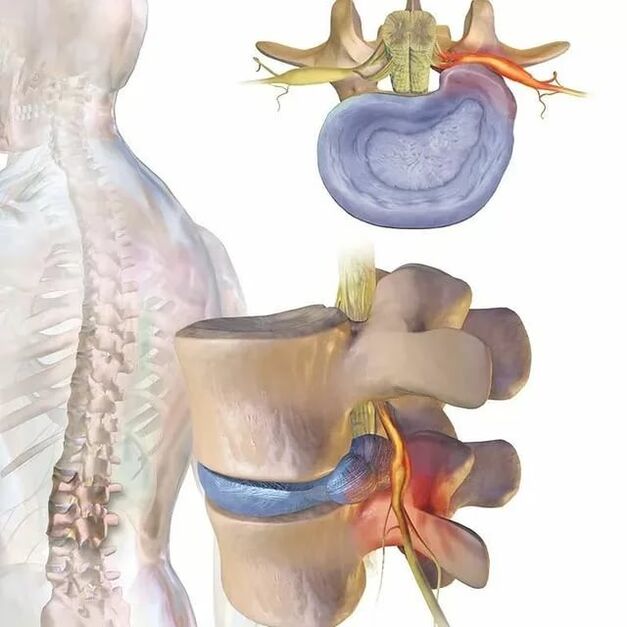
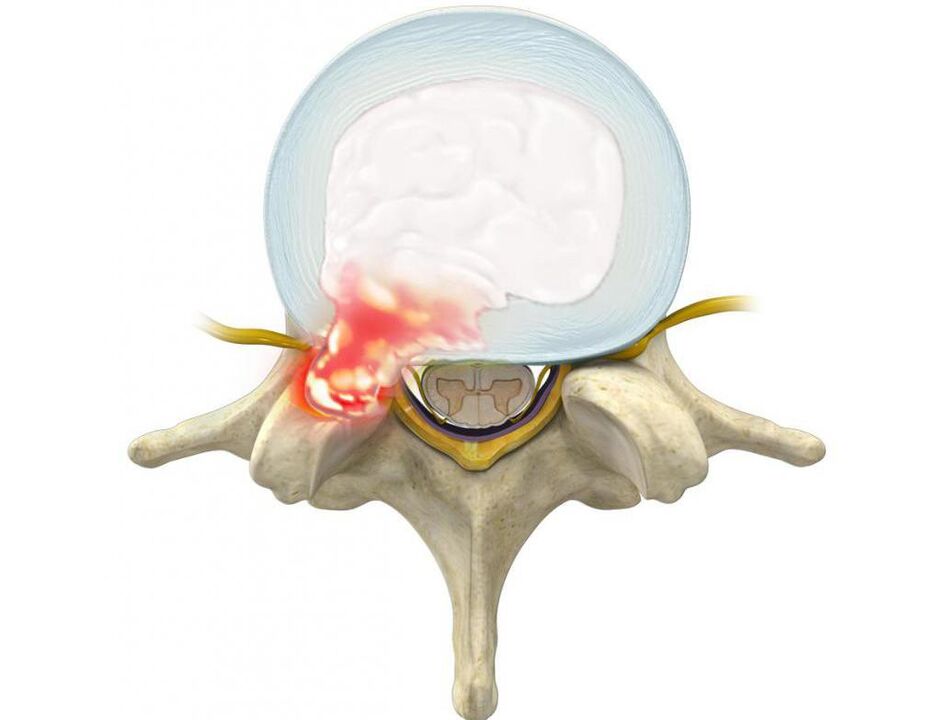
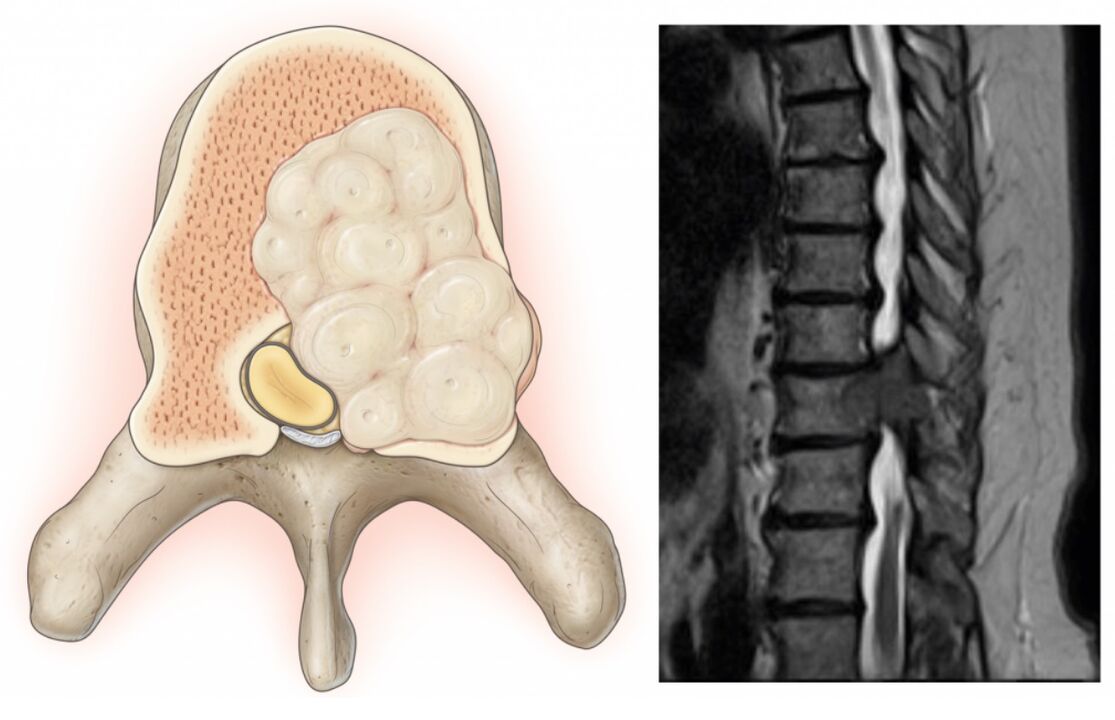
A protrusion is a protrusion of the disc while maintaining the integrity of its outer skin, called the annulus fibrosus. While maintaining the influence of provoking factors over time, the fibrous annulus fibers do not withstand the load and pressure of the internal contents of the disc (nucleus pulposus) and rupture. As a result, the nucleus extends beyond the physiological position of the intervertebral disc. At the same time, the spine in the lumbar region is constantly sore or pain radiates to the legs, and discomfort increases with sudden movements, bending, lifting heavy objects, straining, coughing, sneezing, laughing, as well as with prolonged sitting. one position, walking, standing.
Often, patients with bulges and hernias that have already formed unconsciously assume a forced posture, leaning slightly toward the healthy side. In this case, pain in the spine in the lumbar region can reach a high intensity, depleting a person's work capacity. In such a case, he had to adhere to a bed rest, and to relieve the pain, he tightened the bent leg and brought it to the abdomen.
Often, bulges and hernias form toward the spinal canal, where the spinal cord (cauda equina) and the nerve roots that branch from it pass. The latter passes through natural openings in the vertebral body and branches further into the lumbar plexus, which is responsible for the preservation of the lower legs and various organs (including the genitals).

Therefore, often with long-term osteochondrosis, the formation of hernias in the lumbar region, pain in the spine is gradually not only intensified, but also compounded by other disorders. If a deformed disc or soft tissue swells as a result of the inflammatory process squeezing the spinal roots that pass through it near them, a neurological disorder occurs. Therefore, pain in the spine in the lumbar region can be aggravated by radiating to the buttocks, groin, front, inner, outer thighs, lower legs and feet. It depends on the type of nerve root to be affected, that is, on the degree of pathological changes of the spinal movement segment will be observed. Also, in the corresponding zone on the lower part of the foot, sensitivity disturbances can be observed in the form of a feeling of crawling, numbness, changes in susceptibility to temperature, pain, tactile stimuli and limited mobility.
Changes in the height and function of the disc that arise in osteochondrosis and its complications lead to damage to the articular apparatus of the spine, as well as degeneration of the vertebral body itself. The result is the development of spondylosis, i. e. calcification of the anterior longitudinal ligament and the formation of cartilage growth on the surface of the vertebral body (osteophytes). They can not only injure the surrounding tissues and squeeze the roots of the spine, causing severe pain in the spine, but also grow together. As a result, adjacent vertebral bodies are combined into one whole, which dramatically limits mobility in the lower back.
Osteochondrosis can be accompanied by reactive changes in the vertebral body, in particular, reactive aseptic spondylitis, which leads to osteosclerosis. This is accompanied by compaction of bone tissue and dramatically increases the likelihood of vertebral fractures.
Facet joint disease
Pathology of the facet joints or facets of the lumbar spine, in particular their arthrosis, can also cause pain in the spine in the lumbar region, including severe pain. Although more often the pain is painful and localized deep inside. Their appearance is due to the fact that their synovial capsules are heavily depleted. In such situations, the pain is usually concentrated directly in the affected area and tends to increase with bending, extension, twisting of the body, prolonged standing. Walking and sitting help reduce their severity. But in some cases, pain can also be given in the groin area, coccyx, as well as the back and outer thighs.
Inflammatory diseases of the spine
Inflammatory diseases of the spine are less common than pathology of the intervertebral discs and facet joints. However, they also hurt the spine. This includes:
- ankylosing spondylitis or ankylosing spondylitis;
- reactive arthritis;
- psoriatic arthritis, etc.
The symptoms of the disease usually occur before the age of 40, and more often at the age of 20 years. This distinguishes them from degenerative-dystrophic pathology of the discs and spinal joints, which often develops after 40 years. In this case, the pain is characterized by a gradual increase in intensity. Moreover, their severity decreased after physical exercise, but did not decrease during rest. Thus, in inflammatory diseases, the spine in the lumbar region is often sore at night and especially strongly in the morning, immediately after sleep.
The most difficult situation is observed with ankylosing spondylitis, and it is he who more often than other inflammatory diseases affects the lumbar region. The term means inflammation of the intervertebral joint with subsequent immobilization due to the formation of dense bone, cartilage or fibrous fusion between the articular bone structures.
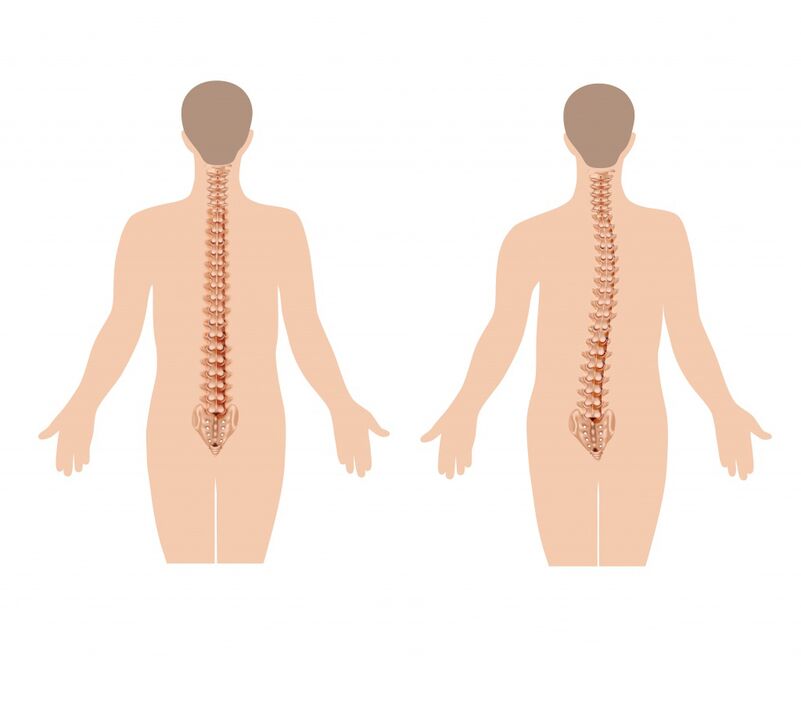
Initially, it is characterized by mild back pain, but over time they gradually spread higher, covering the thorax and then the cervical spine. This is associated with the development of limitations of spinal mobility in all planes, because the spinal column, as a result of the changes that occur, appears to sink in certain cases. Also note:
- alignment of lumbar lordosis (natural curvature of the spine in the lumbar region);
- severity of thoracic kyphosis, which gives rise to hump;
- back muscle reflex tension;
- progressive severity of mobility limitation due to involvement of facet joints in pathological processes and hardening of the intervertebral disc;
- morning stiffness for an hour or so.
In 10–50% of patients, inflammation of the iris (iritis), cornea (keratitis), mucous membranes (conjunctivitis), iris and ciliary body of the eyeball (iridocyclitis) is observed.
The progression of ankylosing spondylitis leads to the fact that an increase in the number of joints in the pathological process. As a result, the patient is forced to acquire a pose called applying. This means obvious kyphosis of the thoracic spine, tilt of the upper body downwards, bending of the knee with a sharp limitation of the range of motion in the chest, which affects the depth of breathing.
The rate of disease progression depends on the adequacy and completeness of treatment.
Vertebral compression fractures
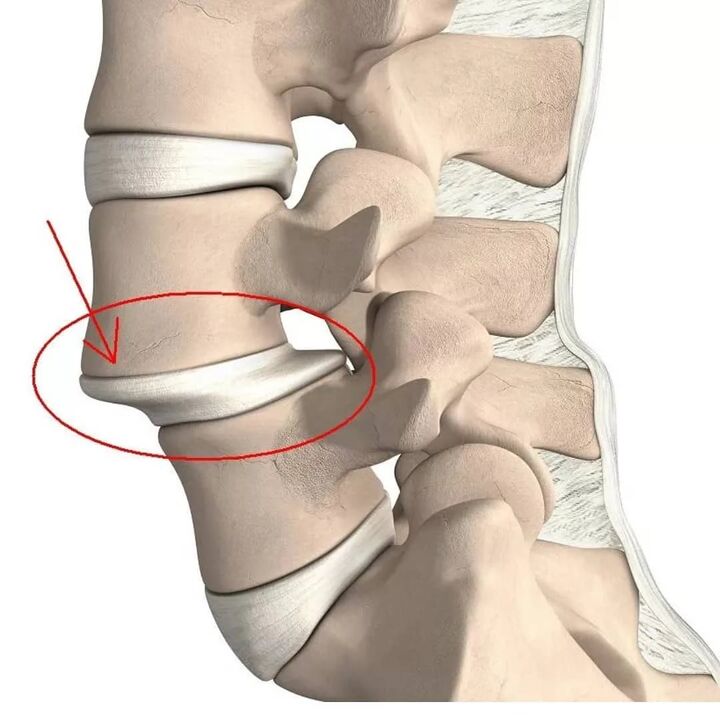
A compression fracture is the flattening of the vertebral body, as a result of which it becomes wedge -shaped. This leads to anatomical disorders of the spine, can trigger trauma to the spinal cord and its roots, and also be a trigger factor for the rapid development of degenerative-dystrophic changes.
Lumbar vertebrae 1 and 2 are more susceptible to injury, as they take the greatest axial load.
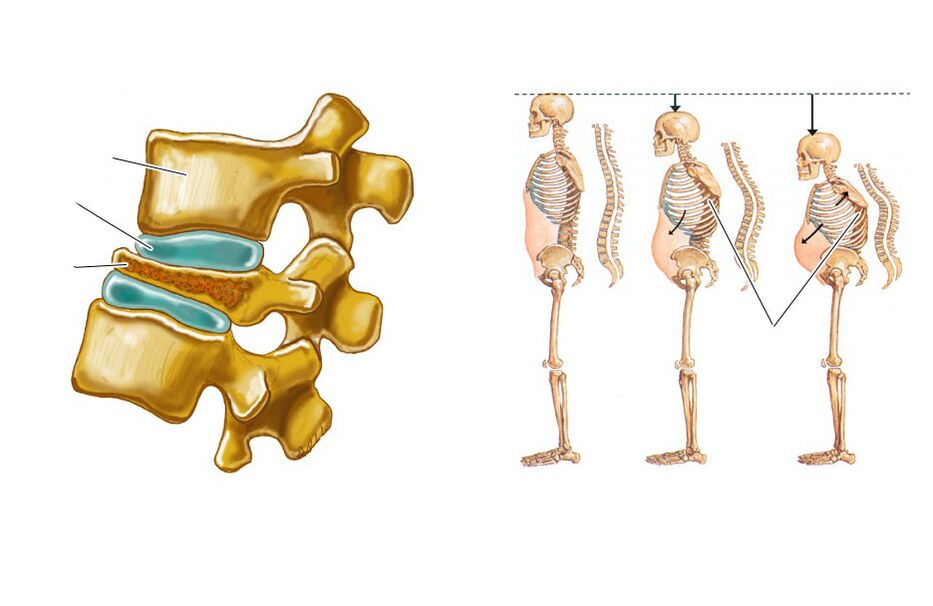
Spinal compression fractures often occur in the elderly due to the development of osteoporosis, which is a decrease in bone density. In such cases, to get injured, it may be enough not only a slight fall, but also heavy lifting, unsuccessful movements.
The pathology is characterized by the presence of pain in the spine, which limits movement, increased by sitting, movement and attempts to raise the leg straight up. It usually lasts 1-2 weeks and then gradually decreases over 2-3 months. In some cases, there is radiating pain at the apex of the iliac and hip bones. A decrease in the height of the fractured vertebra gives rise to an increase in lumbar lordosis, which also contributes to the occurrence of painful sensations.
If the fracture is not diagnosed in a timely manner, a decrease in vertebral height leads to a change in posture, a decrease in growth. This creates reflex tension and shortens the spinal muscles, which causes chronic back pain and requires prolonged rest.
Neoplastic lesions of the spine
Spinal neoplastic lesions mean the formation of benign and malignant tumors in it, as well as metastases, the source of which is neoplasms of other organs. This is much rarer than intervertebral disc pathology, facet joints, ankylosing spondylitis, and even compression fractures, i. e. only in 1-2% of patients with back pain. But such lesions require diagnosis and treatment as early as possible.
The characteristics of neoplastic lesions of the spine, in addition to the pain in them, are:
- increased body temperature, including up to subfebrile values;
- unreasonable weight loss;
- inability to find a comfortable body position;
- the presence of pain at night;
- severe pain in the spine;
- inability to relieve pain with conventional analgesics.
Even if you have 1 or 2 of these symptoms, you should make an appointment with your doctor right away.
In the same way, the following may appear:
- Chondroma is a malignant tumor diagnosed in 20% of patients with spinal cancer lesions. Often it forms in the sacrum and can occur in people of any age and gender.
- Young sarcoma - occurs in 8% of patients with neoplastic lesions of the spine. More common in young men.
- Chondrosarcoma is a malignant neoplasm, which accounts for 7-12% of cases. It is more commonly found in middle -aged men.
- Aneurysm bone cysts are benign neoplasms.
- Hemangiomas are more likely to be benign vascular tumors found in 11% of people. It may go undetected for the rest of a person’s life. But it increases the risk of vertebral fractures.
- Another tumor metastasis is a secondary malignant neoplasm. More often, cancers of the breast, prostate, lung, and less often the kidneys, thyroid gland and skin metastasize to the spine.
Diagnostics
If the spine in the lumbar region is painful, it is worth making an appointment with a neurologist or vertebrologist. At the appointment, the doctor initially collects anamnesis, asks questions about the nature of the pain, the circumstances of its occurrence, the duration of its persistence, the presence of other symptoms, lifestyle, etc.
Then the specialist conducts an examination. In his framework, he not only probes the spine, determines the localization of pain, evaluates the gait and posture taken by the patient unconsciously, but also conducts functional tests. With their help, you can detect signs of ankylosing spondylitis, neurological deficits, assess the level of mobility of the spine and obtain other diagnostic data.
Based on this, doctors can already assume the possible cause of the pain syndrome. To clarify this, as well as to determine the degree of damage accurately, instrumental and sometimes laboratory diagnostic methods are also prescribed. Often they use help:
- radiography in frontal and lateral projections, sometimes with functional radiological examination;
- CT - allows better visualization of bone structure, therefore, it is more often used to diagnose spondylosis, fractures, bone tumors, etc. ;
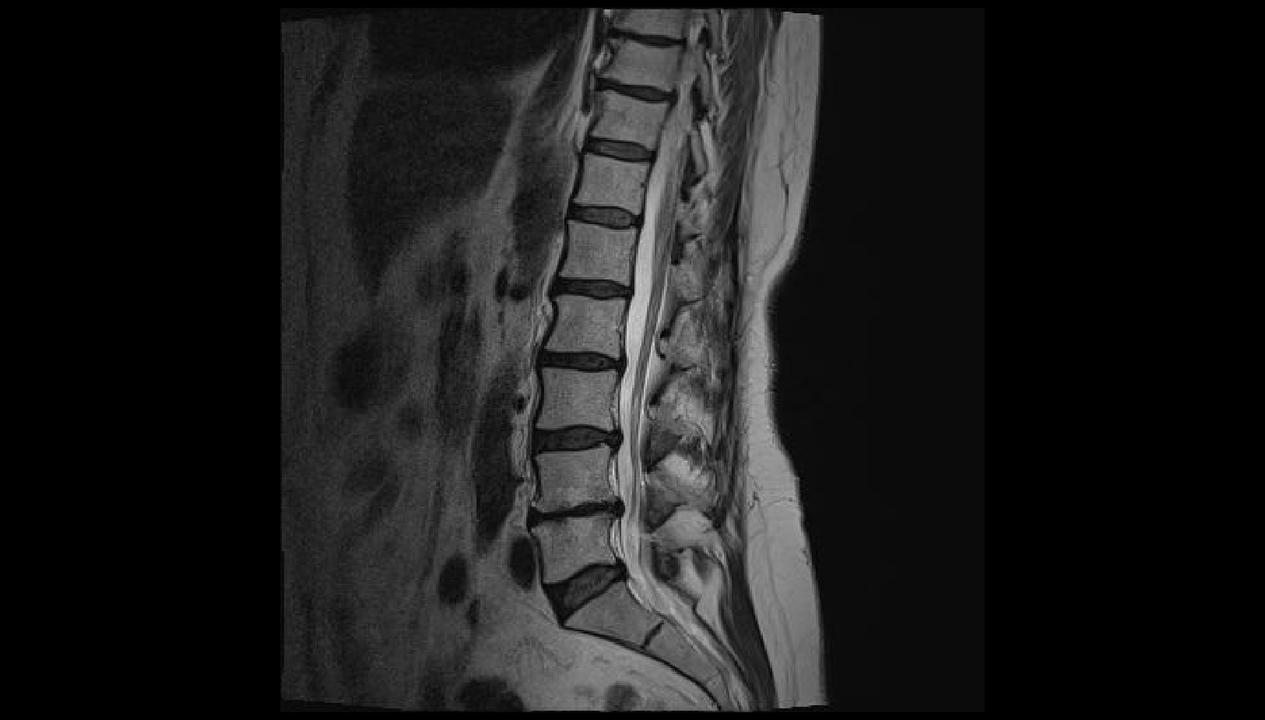
- MRI - makes it possible to assess the state of the structure of cartilage and soft tissue as carefully as possible, therefore it is often used to diagnose osteochondrosis, protrusion, intervertebral hernia, spinal cord lesions, etc. ;
- electromyography - indicated for neurological disorders of unknown origin, as well as to assess the degree of nerve damage;
- radioisotope bone scintigraphy - used to diagnose tumors and malignant metastases;
- X-ray densitometry is the best method for diagnosing osteoporosis;
- myelography - used to detect signs of compression of the spinal cord and cauda equina.

Treatment
For each patient, treatment is chosen strictly individually, and not only on the basis of the diagnosis, but also the nature of the existing corresponding pathology. Nevertheless, the cause of back pain determines the tactics of therapy. It can be conservative or involve surgical intervention.
But the first step is to always direct efforts to relieve pain, especially if it is strong. For this, patients are prescribed NSAIDs, antispasmodics, painkillers. And in severe cases, spinal blockages are performed - injections of anesthetics and corticosteroids at specific points in the spine.
Bed rest is not indicated for all patients. And with intervertebral disc pathology, it may be completely contraindicated, as a decrease in physical activity contributes to the change of acute pain in the spine into chronic.
Conservative or non -surgical treatment is prescribed exclusively for:
- osteochondrosis;
- ankylosing spondylitis;
- facet joint arthrosis;
- mild compression fracture.
It is usually complex and consists of:
- drug therapy, which may include NSAIDs, chondroprotectors, muscle relaxants, immunosuppressants, corticosteroids,
- physiotherapy (UHF, magnetotherapy, laser therapy, traction therapy, etc. );
- Exercise therapy;
- manual therapy.

If the cause of back pain is an intervertebral hernia, protrusions, spondylosis, severe vertebral fractures, tumors, surgery is often indicated. It is also necessary to:
- ineffectiveness of conservative therapy for degenerative-dystrophic changes;
- an increase in neurological deficits;
- instability of spinal movement segments;
- development of complications, especially spinal canal stenosis.
Most modern spinal surgeries are minimally invasive. Thanks to this, intraoperative and postoperative risks are dramatically reduced, the recovery period is shortened and simplified, and its effectiveness is not inferior to more traumatic open surgery. Depending on the disease detected, it may be recommended:
- Discectomy is a surgery indicated primarily for hernias and protrusions, especially those that provoke cauda equina syndrome. It can be performed using a microsurgical instrument through an incision in the order of 3 cm (microdiscectomy) and using endoscopic equipment supplied to the spine through a puncture needle with a diameter of about 1 cm (endoscopic discectomy). When the intervertebral disc is completely removed, it is usually replaced with an implant.
- Vertebroplasty and kyphoplasty - indicated for vertebral compression fractures, hemangiomas and some other diseases. The essence of the operation is to inject rapidly hardened bone cement through a thin cannula into the vertebral body, which strengthens it. With kyphoplasty, it is possible to restore the normal dimensions of the vertebral body, which is important in the event of a serious decrease in their height as a result of a fracture.
- Fixation surgery is used to stabilize the spinal column. For this, different metal structures are used, which usually remain in the patient’s body until the end of life.
Therefore, the spine in the lumbar region can be sore for a variety of reasons. Therefore, with the persistence of prolonged painful sensations, their usual occurrence, increase in pain over time, and even more so the addition of other symptoms, it is important to contact a vertebrologist or neurologist. Early diagnosis will make it possible to detect pathological changes at the stage when it is easiest to overcome it and if the disease is not completely cured, then at least stop its progression and maintain a high standard of living.












































